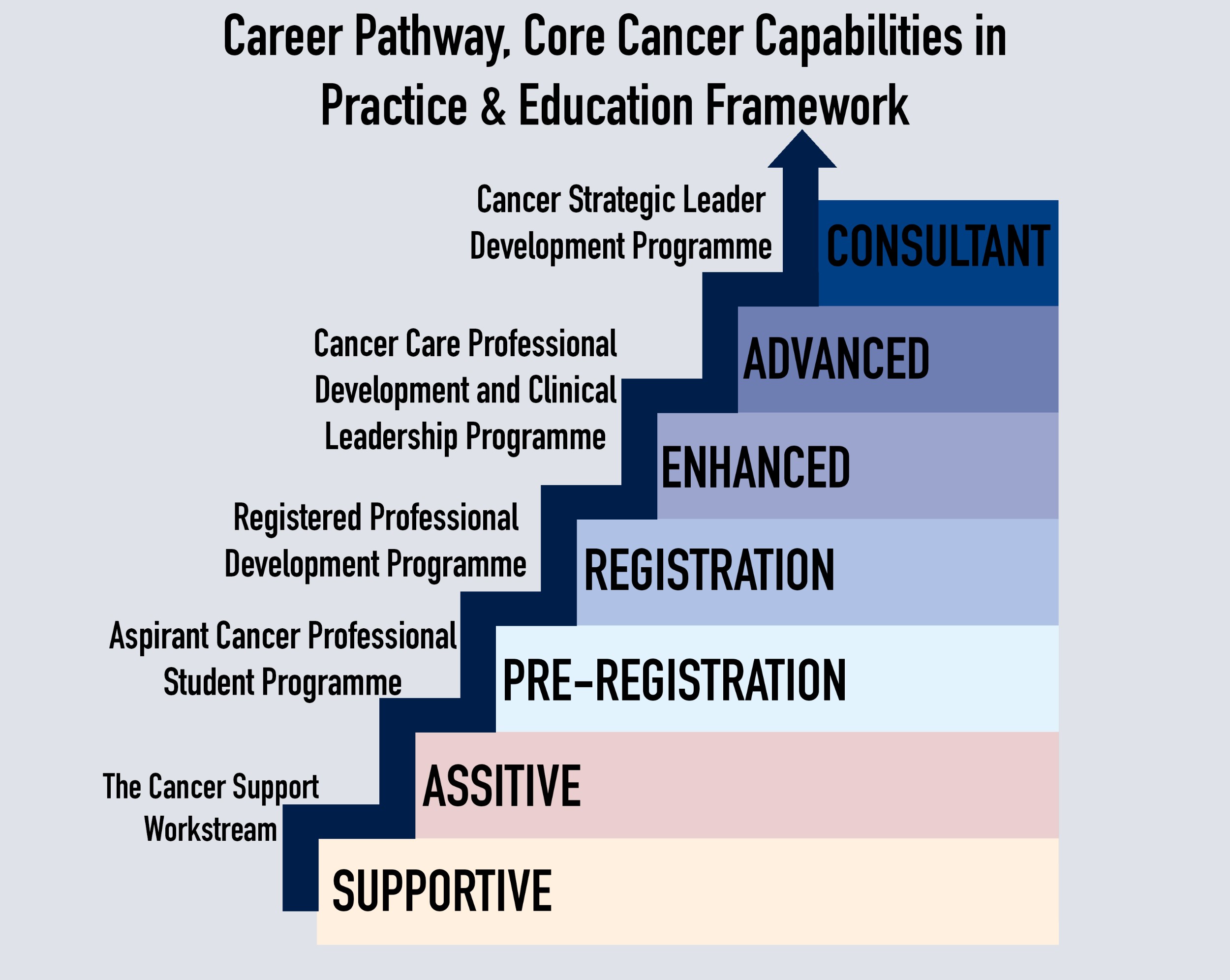
ACCEND Programme workstreams
in relation to levels of practice
On this page you can find everything you need to know about the Aspirant Cancer Career and Education Development programme (ACCEND). The ACCEND programme is for Nurses, Allied Health Professionals and all cancer related support roles.
Below you will find information on the programme, resources, education, training and information about career development pathways for our workforce who support people affected by cancer.
Click the images below to download the SSCA ACCEND Framework Portfolios of Practice, and the ACCEND Framework User Guide!
For further information or any questions please contact us on: rsch.sscaadmin@nhs.net
Latest News:
The Foundations of Cancer Care module for Registered, Enhanced to Advanced levels of practice is now available!

What is ACCEND?
Launched in January 2023, the programme introduced a framework to support the development of the workforce providing care to people affected by cancer. The framework has 3 components:
- Career pathway component; defining levels of practice and demonstrating the knowledge, behaviours, and skills required to be working at each level.
- Core cancer-specific capabilities in practice (CiPs) component; articulating the attributes (knowledge, behaviours, and skills) defined at each level of practice under 7 domains.
- Education framework component; providing core knowledge descriptors for each level of practice and high level learning outcomes and knowledge specifications in relation to the core cancer CiPs and domains.
Levels of practice:
The dedicated healthcare team supporting and assisting in patient care within cancer services consists of a diverse group of professionals. From healthcare assistants and cancer navigators to cancer support workers and AHP support workers, these individuals collaborate seamlessly with the broader multi-disciplinary team. Together, they contribute to the holistic well-being of patients by undertaking a variety of tasks.
Supportive Level:
- Possesses a solid understanding of facts, principles, processes, and general concepts.
- Engages in a wide range of duties with some responsibility, guided and supervised as needed.
- Committed to delivering high-quality, compassionate healthcare.
- Adheres to standards, policies, and protocols within the bounds of their expertise.
- Uses knowledge to make informed decisions, taking ownership of work, and actively reviewing its effectiveness.
Assistive Level
- Foundation of factual and theoretical knowledge is essential.
- Operates independently and collaboratively under the leadership of a registered nurse or AHP.
- Follows defined parameters to deliver care according to agreed plans and protocols.
- Possesses a versatile skill set, catering to local health populations, considering unique perspectives of individuals, families, and/or carers.
- Rooted in providing holistic and personalized care, supporting the entire care process.
- Working whilst guided by standard operating procedures and protocols.
- Actively contributes to service development, making judgments, planning activities, and demonstrating a commitment to ongoing self-development.
- Plays a vital role in enhancing the overall quality of patient care within cancer services.
The pre-registration workforce are individuals who are undergoing training and education to become qualified healthcare professionals. These individuals are in the process of completing their educational and practical training through university programs and clinical placements.
This is when healthcare professionals have completed their education and training that is accredited by a recognised body, they are qualified and licensed to practice within the scope of their specific profession.
At this level, practitioners exhibit the following characteristics:
Education and Accreditation:
- Healthcare professionals gain qualifications and licenses after completing accredited education and training recognized by respected bodies.
Skilled Practitioners:
- Possess a wealth of comprehensive, specialized knowledge—both factual and theoretical—with a keen awareness of boundaries within their expertise.
Problem-Solving and Contribution:
- Creatively leverage knowledge to solve problems, make analytical judgments, and actively contribute to both service and self-development.
Role in Care Provision:
- Lead, coordinate, and evaluate evidence-based, personalized, and compassionate care.
Accountability and Autonomy:
- Assume accountability for actions and delegations, demonstrating the ability to work autonomously or as equal partners with diverse professionals.
Management of Complex Care Needs:
- Expertise extends to providing care for individuals with complex mental, physical, cognitive, and behavioral needs, as well as those at the end of life.
Health Promotion and Prevention:
- Make significant contributions to promoting health, protecting well-being, and preventing illness. Empower people to make choices and manage their own care whenever possible.
Supervisory Responsibilities:
- Take charge of supervising students, staff, or training initiatives, underscoring their comprehensive role in the healthcare landscape.
Practitioners at this level go beyond the basics, acquiring additional skills, knowledge, and experience beyond their initial registration requirements. In this advanced stage, they often step into more specialized roles, embracing increased responsibilities within their professional domain.
At this level, practitioners exhibit the following characteristics:
In-depth Knowledge and Leadership:
- Possess a critical understanding of detailed theoretical and practical knowledge, either as generalists with a special interest or specialists with focused expertise.
- Manage and lead responsibilities within their role.
Specialist Skills and Capabilities:
- Acquire specialist knowledge, skills, and capabilities directly related to their sphere of practice.
Collaborative Patient Care:
- Consult with patients, their families, and the multi-professional team to conduct assessments of patient needs.
- Devise and evaluate complex care plans through a comprehensive approach.
Clinical Problem Solving:
- Evaluate and analyze clinical problems using their in-depth knowledge, seeking and applying relevant evidence, enhanced techniques, interventions, and equipment to make informed clinical decisions.
Adaptability and Innovation:
- Deliver enhanced clinical care amid continual change, challenging environments, different models of care delivery, innovation, and rapidly evolving technologies.
- Utilize analysis and deep knowledge to manage complex interventions effectively.
Educational Role:
- Teach and advise patients and their families on how to manage their conditions or support the multidisciplinary team in doing so.
Research and Development:
- Participate in clinical audits and research projects, implementing changes as required.
- Contribute to the development and updating of practice protocols, guidelines, and procedures at the local level.
Adherence to Protocols and Boundaries:
- Work within national and local protocols where available.
- Recognize the boundaries of their practice, knowing when and to whom patients should be referred.
Delegation and Accountability:
- Delegate work to other members of the multidisciplinary team, taking accountability for the delegated activity.
Initiative and Creativity:
- Demonstrate initiative and creativity in finding solutions to problems.
Team Performance and Service Development:
- Have some responsibility for team performance and service development.
- Consistently undertake self-development, contributing to the continual advancement of their professional skills.
This level involves professionals who have pursued further education, training and often certification. Advanced practitioners have expanded scope of practice, allowing them to take on more complex clinical tasks.
Practitioners at this level not only combine advanced clinical skills but also intertwine research, education, and clinical leadership seamlessly within their scope of practice. Their characteristics include:
Holistic Expertise:
- Merging advanced clinical skills with research, education, and clinical leadership.
Critical Awareness:
- Possessing a critical awareness of knowledge issues within the field and at the interface between different fields.
Innovation and Responsibility:
- Being innovative and shouldering responsibility for developing and changing practice and/or services in a complex and unpredictable environment.
Demonstrated Expertise:
- Demonstrating expertise within their defined scope of practice.
Independent Clinical Management:
- Managing clinical care independently at the highest level, overseeing the entire process from an individual's presentation to the conclusion of the episode. This may include admission, referral, discharge, or care at home.
Collaboration Across Boundaries:
- - Collaborating as an integral part of the broader health and social care team and transcending traditional professional boundaries.
Regional Leadership:
- Working across the service, network, and/or regionally, leading and influencing practice development and service improvements.
Adherence to National Standards:
- Satisfying all the requirements of their nation to be recognized as an Advanced Practitioner.
This level not only represents a culmination of advanced skills but also a commitment to holistic, innovative, and impactful practice within the ever-evolving healthcare landscape.
This is the highest level of practice and often involves professionals who have achieved a significant level of expertise in their speciality. Consultants are recognised leaders in their field and may be involved in teaching, research, and leading clinical teams.
Practitioners at this level exhibit the following characteristics:
Cutting-Edge Specialized Knowledge:
- Requiring highly specialized knowledge, some at the forefront of their field, serving as the bedrock for original thinking and/or research.
Leadership and Analytical Prowess:
- Being leaders with substantial responsibility, equipped with the ability to research and analyze intricate processes.
Driving Service Improvement and Innovation:
- Holding responsibility for service improvement, development, and innovation.
Pioneering Research and Knowledge Generation:
- Generating new knowledge about the best treatment and care by actively seeking and implementing evidence to enhance health and care outcomes.
Strategic Leadership and Change Management:
- Applying expert knowledge and leading strategic change across entire systems through ongoing clinical development and research.
Leading at the 'Leading Edge':
- Operating at the ‘leading edge’ of their profession, developing and consolidating clinical expertise through interdisciplinary research and clinical leadership.
Knowledge Transfer and Mobilization:
- Leading the transfer and mobilization of new knowledge, utilizing implementation science methods to address high-priority questions related to service delivery.
Transformational Leadership in Patient Care:
- Transforming the way care is developed and delivered, leading partnerships with patients, the public, clinical academic experts, and other stakeholders to make improvements locally, nationally, and internationally.
Diverse Responsibilities:
- May encompass considerable clinical and/or management responsibilities, accountability for service delivery, or a leading role in education or commissioning.
Nationwide Recognition:
- Satisfying all the requirements of their nation to be recognized as a consultant practitioner.
At this level, practitioners not only represent the pinnacle of clinical expertise but also epitomize leadership, innovation, and a commitment to shaping the future of healthcare on a broad scale.