The NHS Long Term Plan for Cancer states that "where appropriate every person diagnosed with cancer will have access to personalised care, including a needs assessment, a care plan and health and wellbeing information and support".
A 'one-size-fits-all' health and care system simply cannot meet the increasing complexity of people’s needs and expectations. Personalised care is based on ‘what matters’ to people and their individual strengths and needs.
Our work includes working in partnership with health care professionals to develop best practice guidelines.
We are working with commissioners and providers of cancer services to ensure the four main personalised care interventions are available for all cancer patients. These four are:
An Holistic Needs Assessment (HNA) is offered following a cancer diagnosis and provides an opportunity to ensure people’s physical, practical, emotional and social needs are identified and addressed at the earliest opportunity.
We have produced an Holistic Needs Assessment (HNA) guidance which describes the agreed expectations for implementing HNAs in acute settings across the Surrey and Sussex Cancer Alliance. It explains what an HNA is, who should be offered one and how it should be completed. This guidance will help promote a consistency of approach in the offering and administration of HNAs by cancer units and centres.
Macmillan has also created the Macmillan Holistic Needs Assessment e-learning to help and support key workers in the delivery of effective and supportive HNAs and care planning. Find out more about Holistic Needs Assessments.
We have created a guidance and resource pack for healthcare professionals in collaboration with a number of partners and patient representatives. It provides top tips for you to deliver virtual health and wellbeing support, outlines the key elements to include, and also provides details of resources available for patients across Surrey and Sussex. View the Virtual Health and Wellbeing Guidance and Resource Pack.
The pack covers accessible information about emotional support, coping with side effects, financial advice, getting back to work and making healthy lifestyle choices. This support will be available before, during and after cancer treatment. This may be via group or one-to-one interventions and could be delivered in person or remotely.
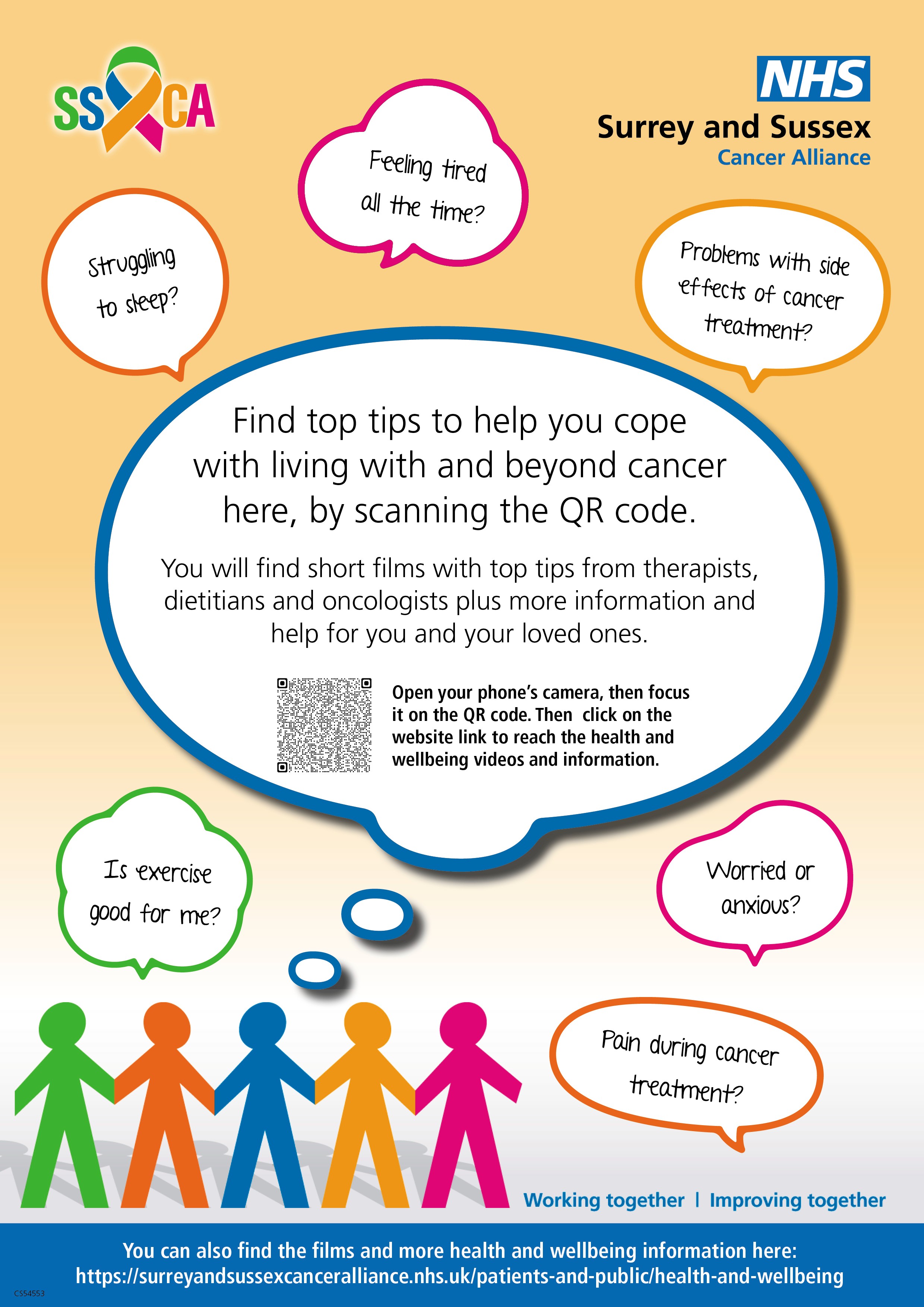 You can also find Health and Wellbeing information for patients on the Health and Wellbeing page. It includes short films from healthcare professionals giving top tips on subjects such as improving sleep and exercising through treatment, managing side effects and pain, and coping with fatigue. Please download this health and wellbeing poster and display in your waiting rooms and all areas where patients living with and beyond cancer are likely to be. It has a QR code which means they can quickly access the advice on our health and wellbeing page.
You can also find Health and Wellbeing information for patients on the Health and Wellbeing page. It includes short films from healthcare professionals giving top tips on subjects such as improving sleep and exercising through treatment, managing side effects and pain, and coping with fatigue. Please download this health and wellbeing poster and display in your waiting rooms and all areas where patients living with and beyond cancer are likely to be. It has a QR code which means they can quickly access the advice on our health and wellbeing page.
Macmillan Delivering Virtual Health and Wellbeing Events is a toolkit for professionals to support the delivery of health & wellbeing or information & support events/groups online.
Cancer Care Map is an online resource to help people living with cancer find care and support services in their local area
Surrey and Sussex Cancer Alliance has produced the first of a suite of updated End of Treatment Summaries (EoTS) to support the care of patients after treatment for cancer.
The first two revised EoTS are for Oesophagogastric and Prostate. All cancer teams across the SSCA footprint have received these EoTS to enable them to be populated with local information and patient details.
An EoTS is a key communication tool to support the patient pathway, acting as a summary of treatment undertaken in secondary care. They should be sent digitally to general practice for uploading to patient health records, at an appropriate point in a patient’s treatment.
An EoTS includes:
- SNOMED codes;
- information about ongoing management and continued medication;
- diagnosis, staging and treatment;
- long-term effects of treatment;
- symptoms that are possible signs of cancer recurrence;
- and any requests for general practice.
The treatment summaries have been produced in partnership with primary and secondary care and patients. Revised EoTS for other tumour pathways will be published next year (2026).
The templates for Oesophagogastric and Prostate EoTS are below, for information purposes only:
End of Treatment Summary - Oesophagogastric
End of Treatment Summary - Prostate
This is an appointment with the patient and GP within 12 months of a diagnosis. It provides an opportunity to raise any new and ongoing concerns. If appropriate, a person can be referred to services or signposted to information and support available in their community and from charities.
Macmillan has produced a guide which provides the knowledge, tips and tools to set up meaningful Cancer Care Reviews at your GP practice, regardless of profession or role. Find the guide here: Personalised-Care-Practical-Implementation-Guide-For-Cancer-Care-Reviews (macmillan.org.uk)
Macmillan has also compiled 10 top tips to help primary care professionals carry out effective Cancer Care Reviews: 10 top tips for primary care: Effective Cancer Care Review

